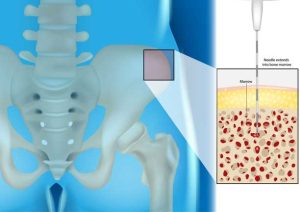
Bone Marrow and its Healing Properties: Understanding BMAC Treatment (Bone Marrow Aspirate Cell Concentrate Treatment)
Let’s say you tore a ligament skiing or have just undergone a procedure to repair torn cartilage, you might have a touch of arthritis in your shoulder that is bothering you. Your doctor may recommend a procedure called BMAC or Bone Marrow Aspirate Stem Cell Concentrate treatment to help the healing process along. It sounds a little wordy, but it just might be the last piece of the puzzle in overcoming an injury. What is BMAC? By now, many people have some awareness that the medical world is able to use the body’s bone marrow to harvest stem cells, which can be used in specific ways to heal the body. One such element is Bone Marrow Aspirate Stem Cell Concentrate (BMAC), which is a component of your bone marrow that contains growth factors and anti-inflammatory proteins, which have been shown to promote bone and soft tissue healing as well as reduce symptoms of pain related to injuries, tendinitis and arthritis. What injuries can be helped by Bone Marrow Aspirate Cell Concentrate treatment? Chronically painful areas of the body often do not have adequate blood supply, healing potential, and regenerative cells to repair the damage. That’s where BMAC is highly useful. BMAC, applied to the right area, can provide a rich supply of regenerative cells with the ability to replicate into various types of tissue. It has tremendous potential for patients with moderate to severe orthopedic conditions or injuries, and is often used to treat severe arthritis in the shoulder, knee, and hip. How is BMAC treatment performed? This procedure is typically done under anesthesia and consists of simple needle punctures to the affected joint. Stem cells are collected from the bone marrow by inserting a needle into the intramedullary (innermost) space of the bone. The aspirated blood is then centrifuged